Cardiovascular disease (CVD) remains the leading cause of death globally, yet certain populations are disproportionately affected. According to Dr. Lee Kirksey, a Cleveland vascular surgeon and advocate for health equity, low-income individuals, women, racial minorities, and rural Americans face significantly higher rates of heart attacks, strokes, and limb loss. These disparities arise from a combination of health risk factors, including obesity, diabetes, high cholesterol, and smoking, coupled with systemic barriers such as inadequate health insurance coverage.
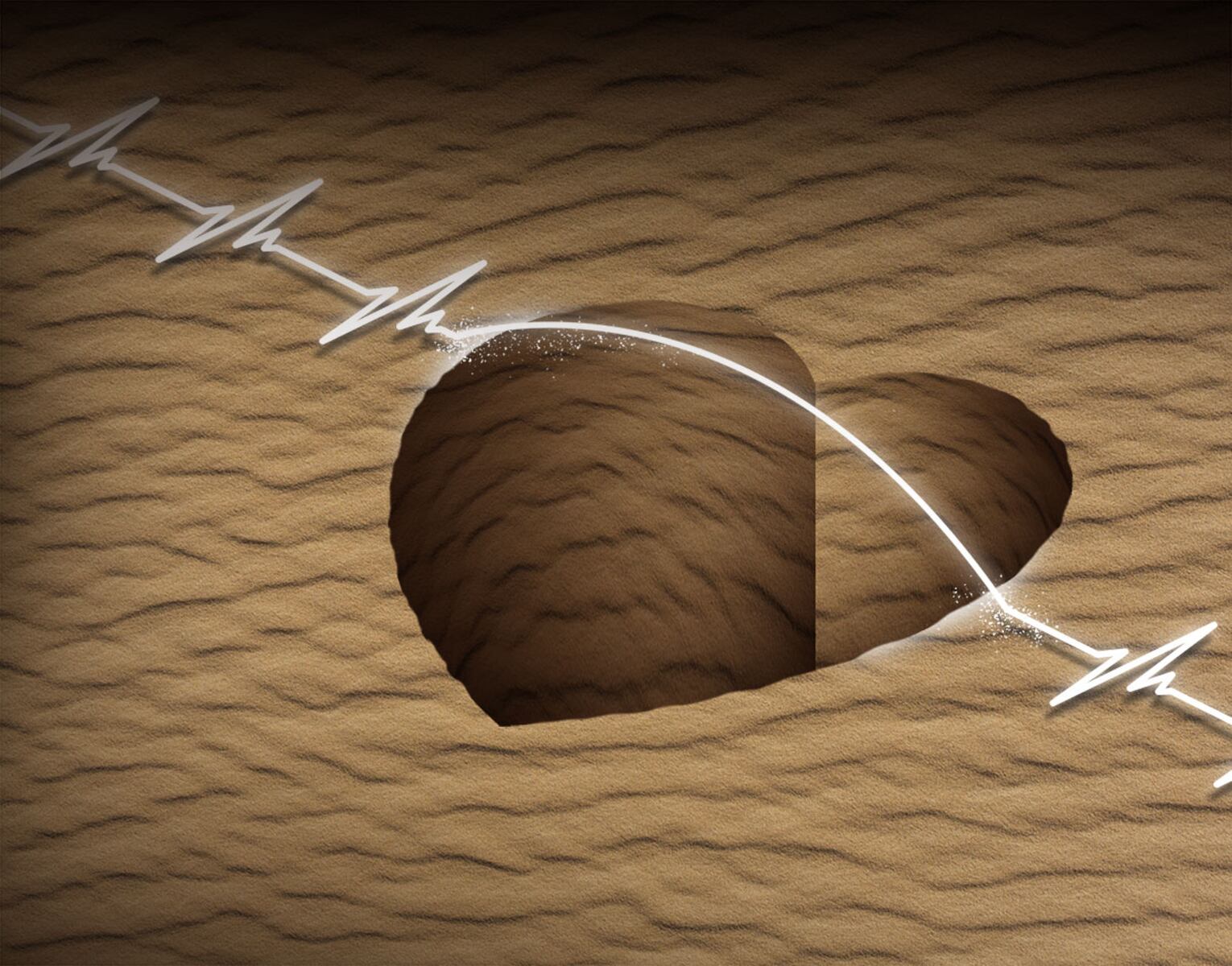
The term “Cardiovascular Desert” has emerged to describe areas where access to cardiologists, primary care physicians, and hospitals is severely limited. Dr. Kirksey, who grew up in the rural community of Alliance, Ohio, emphasizes that geographic distance from advanced medical care can lead to dire health outcomes. A location that appears close to major medical centers on a map often translates into long travel times, missed workdays, and financial losses for residents. This has contributed to a widening gap in life expectancy between rural and urban populations since the 1990s.
The situation has worsened due to economic decline in areas like Ohio, particularly following the manufacturing exodus in the 1990s. Dr. Kirksey cites the phrase by political consultant James Carville: “It’s the economy, stupid!” A lack of economic opportunities exacerbates health disparities, making it increasingly difficult for residents in these “deserts” to access necessary healthcare services.
Recent legislative actions, particularly the One Big Beautiful Bill Act (OBBBA), signed into law on July 4, 2025, threaten to deepen these disparities. This law will reduce federal spending on Medicaid by more than $900 billion over the next decade, potentially stripping over 11 million people of their health coverage, including benefits from the Affordable Care Act and the Children’s Health Insurance Program. Additionally, the elimination of the Grad Plus Loan program for medical students may deter individuals from low-income backgrounds from pursuing careers in medicine, worsening physician shortages in underserved areas.
Innovative treatments, such as the medications Wegovy and Ozempic, have shown promise in addressing obesity and diabetes—two critical risk factors for cardiovascular events. However, access to these treatments is inconsistent across different insurance types, often resulting in out-of-pocket costs that can reach $1,000 per month. This financial burden means that the very innovations designed to improve health outcomes are often out of reach for those living in cardiovascular deserts.
Telehealth offers a potential solution to expand access to care. Yet, significant challenges remain, including the need for partnerships with broadband providers to enhance internet connectivity in underserved areas. The “Digital Divide” is a critical barrier, as low digital literacy in vulnerable communities hampers the effective use of telehealth services. Long-term reimbursement strategies from payers are essential to support infrastructure investments and ensure the sustained use of telehealth by providers.
Dr. Kirksey advocates for a multi-faceted approach to address the challenges posed by cardiovascular deserts. This includes political commitment, collaborative partnerships, and targeted strategies to improve healthcare access in affected communities. He remains dedicated to the health of communities like the one where he grew up, underscoring the urgent need to address these health disparities comprehensively.
As discussions around healthcare reform continue, the plight of those living in cardiovascular deserts must not be overlooked. Effective solutions require a collaborative effort among policymakers, healthcare providers, and communities to ensure equitable access to vital health services.